Osteoporosis and Osteopenia
August 2, 2023
Designing an Effective Non-Drug Treatment Program
Summary
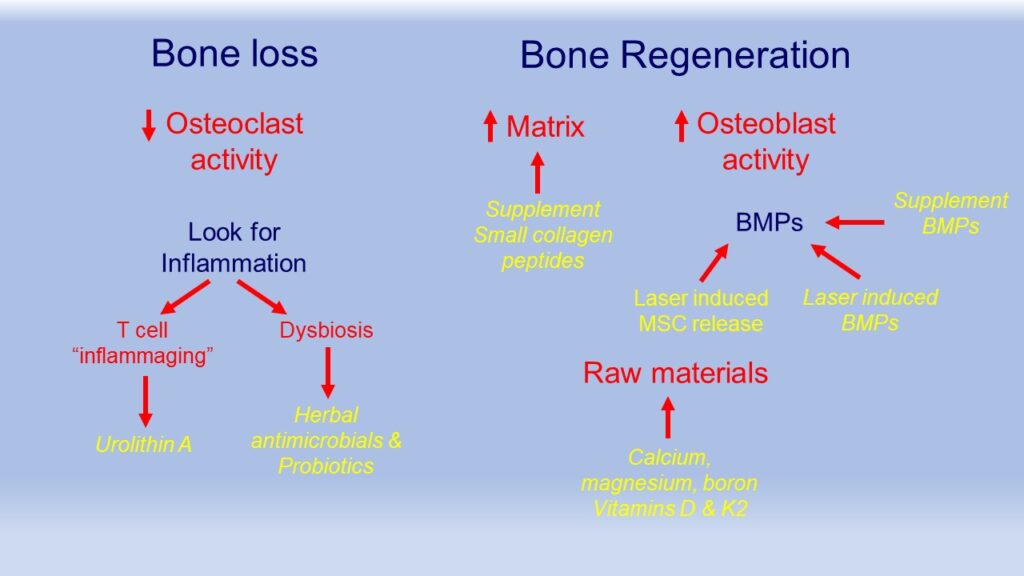
As we have discussed in this series, osteoporosis and osteopenia are common with age. Simply supplying the building components of bone, minerals and vitamins D & K2 are the standard concept of non-drug treatment, yet the research demonstrating benefit once disease is present is rarely helpful. The maintenance of bone density is highly dependent upon balanced activity between osteoclasts which remove old bone and osteoblasts which build bone. There is a gradual shift in this balance with more osteoclastic activity inducing bone loss and less osteoblastic activity building bone beginning about 30 years of age and accelerating after the age of 50. (See Osteoporosis – 1st blog post)
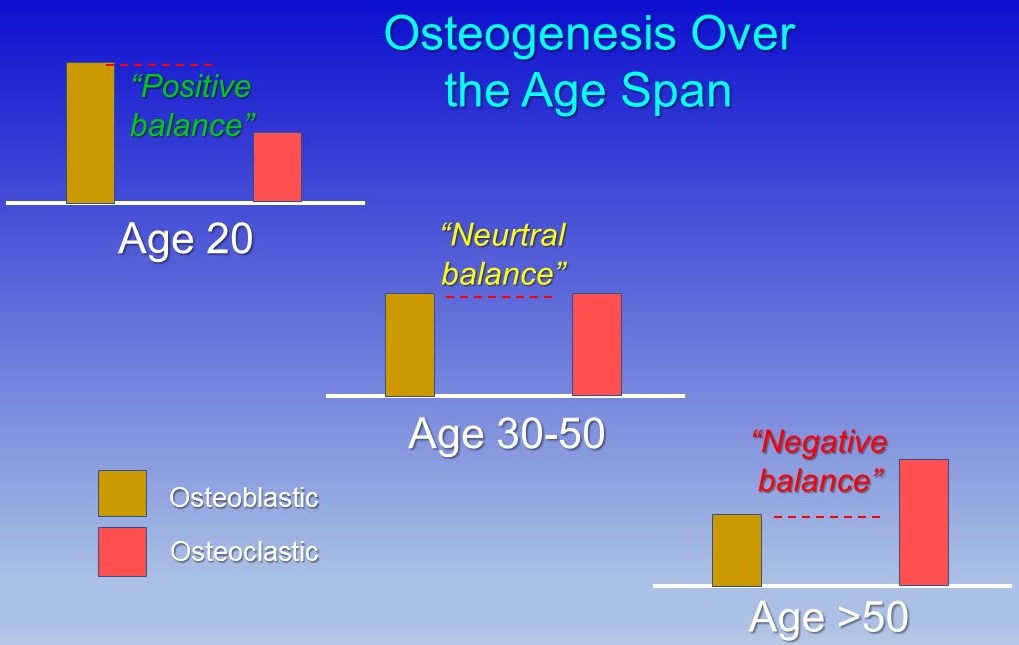
This shift in bone cell activity is related to the progressive increase in inflammation that occurs with age termed “Inflammaging”. (Inflammation and bone loss – 2nd blog) Inflammation increases the activity of osteoclasts promoting bone loss.
The progressive age related inflammation can be caused by one or both of two processes. The first is dysfunctioning immune cells called T cells which are involved in generating inflammation to fight infection or to begin repair in injury. These cells have several mitochondria, the engines that take dietary energy sources such as glucose and convert them into ATP which is cell energy.
As these mitochondria begin to lose function, they have difficulty completing this conversion and produce high numbers of free radicals which trigger inflammation. These aging mitochondria should be removed by a process called autophagy where they are encapsulated in a membrane and dissolve. Autophagy weakens with age. Recent research has shown that a metabolite, urolithin A, which is produced from foods such as strawberries and walnuts by the gut microbiome stimulates autophagy. Direct supplementation of urolithin A has been shown to restore mitochondrial function and reduce this inflammation. (Inflammation and bone loss – 2nd blog)
The second potential source of excessive inflammation is an imbalance in the gut microbiome called dysbiosis. The gut microbiome numbers about 100 trillion organisms from about 1000 species. The young microbiome ferments soluble dietary fiber producing short chained fatty acids which are anti-inflammatory. Extensive study has shown the microbiome becomes less diverse with age with more bacteria that causes inflammation and fewer that reduce it, dysbiosis. (Inflammation and bone loss – 2nd blog)
Dysbiosis is thought to be related to higher numbers of antibiotic exposures with age as therapy or in food passthrough. Antibiotic exposure in infancy is particularly predisposing as that is a key period of microbiome development. Dysbiosis can be helped with herbal antimicrobials to remove inflammatory bacteria and probiotics to restore a healthy population improving inflammatory control.
The second area of attention is in restoring osteoblastic activity in bone building. Osteoblasts don’t live as long as we do and new ones need to be replenished by mesenchymal stem cells (MSCs) which migrate to different tissues from bone marrow in long bones. To do so they need a homing signal to know which type of cells need to be replenished. The remaining osteoblasts in bone secrete bone morphogenic proteins (BMPs) which draw stem cells to that tissue. As osteoblast numbers decline over time loss of this homing signal compounds the problem as fewer stem cells migrate to that tissue. (Activating osteoblasts for bone building – blog 3)
Two therapies can help restore the stem cell regeneration of osteoblasts, BMPs supplements and laser therapy. Supplements of BMPs have shown significant improvements in bone density. These can be augmented by infrared laser to the weaken bone as it stimulates BMP release from the remaining resident osteoblasts. This is complemented by infrared laser over accessible bone marrow sites such as the shin bone which increases stem cell release for migration.
With adequate osteoblastic activity, adequate matrix which is the fibrous mesh that the mineralized bone is built on is needed. Matrix is collagen which is the main protein that is part of the structure of every body tissue. Bone matrix requires a very small collagen peptide as does the skin, joint cartilage and tendons. These small collagen peptides are available in supplemental form and help with age related degeneration in all of these tissues. (The piece we omitted, matrix – Blog 4)
Osteoporosis is a complex problem with several parts. It can, however, be helped by careful examination of these parts and appropriate restorative therapies. The diagram below may help to see the flow of this process.