
Osteoporosis
June 13, 2023
Designing an Effective non-drug Treatment Program
The U.S. population as well as that of the developed world broadly is aging. The U.S. population grew 28% from 1985 to 2000. This growth was not evenly distributed between all age groups.
The 15-44 age group experienced no growth over that interval. For every child aging up into this group, one aged out of it. In contrast the 45 to 64 age group increased 70% or about 2 ½ times population growth. The 65 and up age group grew by 60%. This shift to an older population continues today and is projected to for several more decades. A striking quote from aging related researchers perhaps summarizes this best, “By 2050, the world population over 60 years will exceed the size of the global population of young individuals.”(1)
A natural outcome of this demographic shift is a population that has growing numbers of age-related diseases. One of those diseases is osteoporosis. Approximately 20% of the adult population have the disease while more than 1 in 4 women over 64 years have it. Equally alarming is the fact that more than 50% of women >64 years have osteopenia which is in essence an early form of osteoporosis.
The concern with osteoporosis is fragility fracture which is a fracture from either no stress other than weight bearing or from less force than would be needed to fracture healthy bone. Osteoporosis increases fracture risk approximately 70% compared to that in healthy bone. Osteopenia is not benign and increases the risk 31% compared to healthy bone.
As with many diseases, prevention of osteoporosis is the best course with ongoing weightbearing exercise; adequate intake of minerals, Vitamin D and Vitamin K; and a low inflammatory lifestyle of diet, gut health and other factors. The inflammation part may be the least appreciated by the public, and we will elucidate that in a segment of this blog series. The difficulty with prevention is that it has to be done in the 3-4 decades before bone loss occurs, yet it is often not addressed until the disease is present when it is marginally helpful.
The intake of the above nutrients needed for bone repair and health has only a small therapeutic value once significant bone loss is present. This relates to the disease process itself which is an imbalance in the bone removal cells (osteoclasts) and the bone forming cells (osteoblasts).
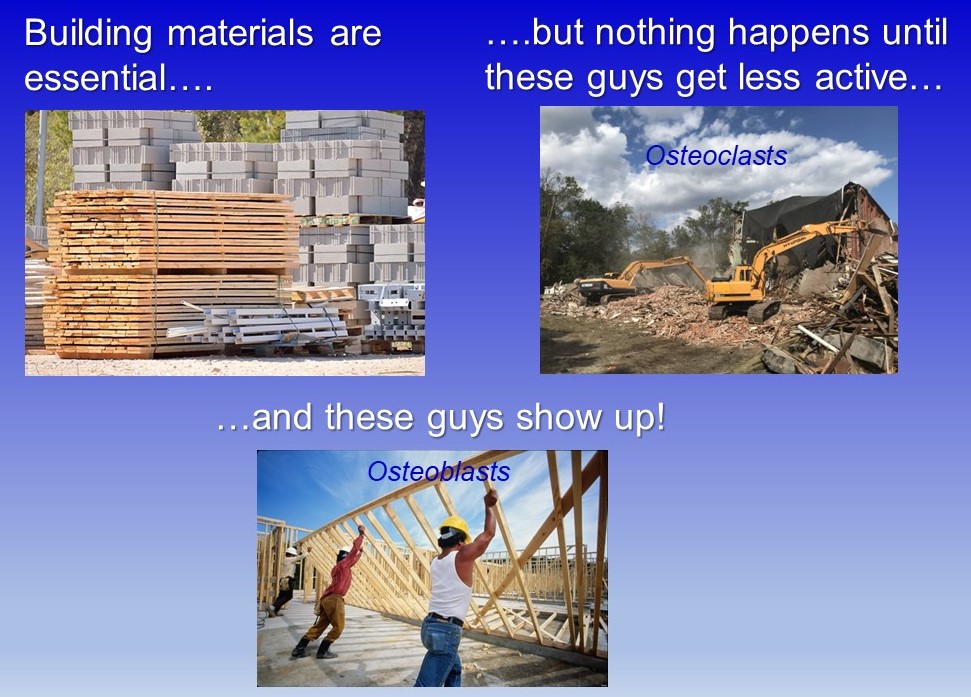
A good analogy to understand this is looking at the process of tearing down a house that is very damaged and building a new one. Healthy bone is always tearing down (osteoclasts) and building back (osteoblasts). When stress on bone changes, osteoclasts remove bone from non-stressed areas and osteoblasts build it in stressed areas. Osteoclasts are analogous to the demolition crew to tear down the damaged house. Osteoblasts then have to build the new one using minerals, vitamin D and K.
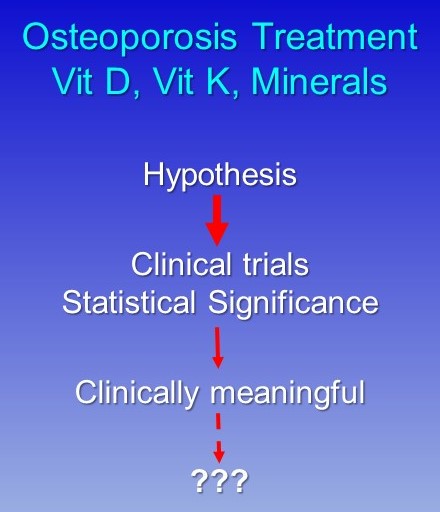
Simply supplying those materials without having the builders (osteoblasts) show up is futile. Similarly, not quieting the demolition crew (osteoclasts) will just tear down the new. Having adequate materials is important but only if the cell activity is normalized. Calcium and vitamin D is the most common recommendation for non-drug treatment of osteoporosis to reduce fracture risk, but it helps only marginally once bone loss is present. Studies have shown that supplementation of these nutrients can make a statistically significant change in bone density, but there is doubt that this change is clinically meaningful. A 2020 study found that this supplementation improved bone density 1%. While the research analysis showed that this was statistically significant or occurred fairly uniformly, it is not clinically meaningful.
An example of these terms might be taking chronic back pain patients who have a pain score of 8 of 10 on a VAS scale. If some treatment showed fairly uniformly that it lowers A VAS scale to 6.9 of 10 that would be statistically significant. Clinically meaningful would mean the majority of patients reported that that made a meaningful change in their function, employability, and other measures. This answer is likely to be no.
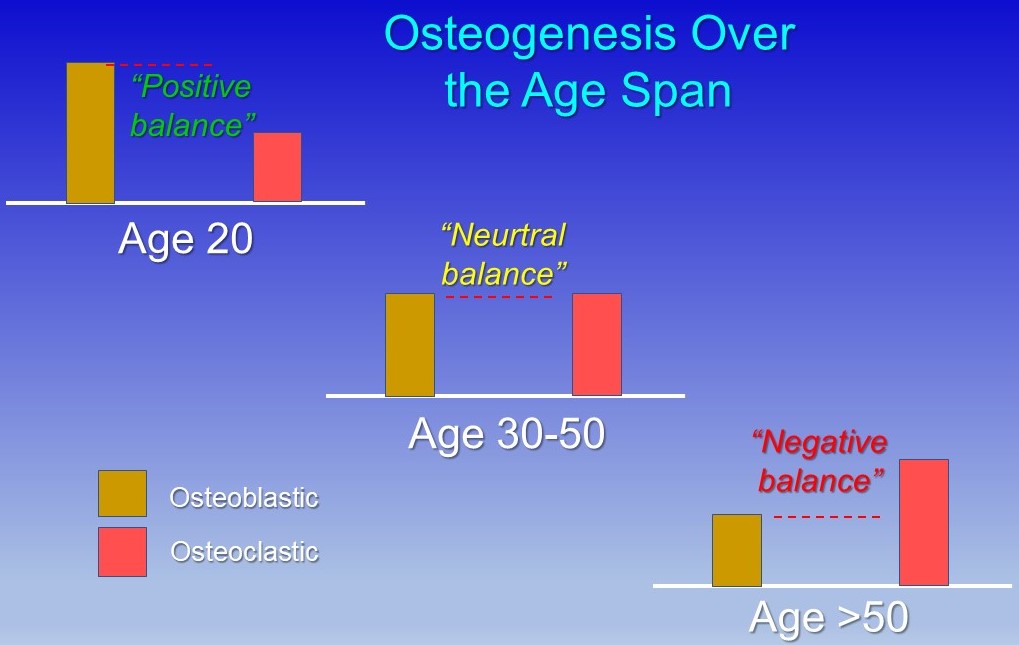
During aging, osteoclasts tend to become progressively more active, and osteoblasts become less active resulting in higher bone removal and weakened bone repair or building. A major stimulus to osteoclastic activity is inflammation which tends to progressively increase from middle age on.
In the next blog in this series, we will discuss this inflammation during aging which has been termed inflammaging. There are many modifiable lifestyle factors that drive it and good non-drug therapies which can mitigate it. The goal is to minimize the increased osteoclastic activity. Then in the subsequent posts we will discuss increasing osteoblastic activity, stimulating stem cell migration to replenish osteoblasts and the other pieces of this process. Stay tuned….
1) Sato Y, Yanagita M. THE UNPRECEDENTED ERA OF AGING. Inflammation and Regeneration (2019) 39:15.
2) Weaver et al. CALCIUM PLUS VITAMIN D SUPPLEMENTATION AND RISK OF FRACTURES: A UPDATED META-ANALYSIS FROM THE NATIONAL OSTEOPOROSIS FOUNDATION. Osteoporosis Int, 2016;27:367–376.
3) Reid IR, Bolland MJ. CALCIUM AND/OR VITAMIN D SUPPLEMENTATION FOR THE PREVENTION OF FRAGILITY FRACTURES: WHO NEEDS IT. Nutrients, 2020;Apr;12(4):1011.