
Osteoporosis
July 13, 2023
Designing an Effective Non-Drug Treatment Program
Part 3 – The Piece We Omitted!

In writing this summary putting all of the pieces of osteoporosis treatment together, I realized that a piece of the process was left out in the last blog. That piece is insuring/restoring bone matrix. Bone matrix is the fibrous mesh that supports the mineralized bone similar to how rebar is used to strengthen concrete or the mesh that stucco is applied to. Drugs that promote mineral deposition such as bisphosphonates must have an adequate matrix to hold the mineral structure.
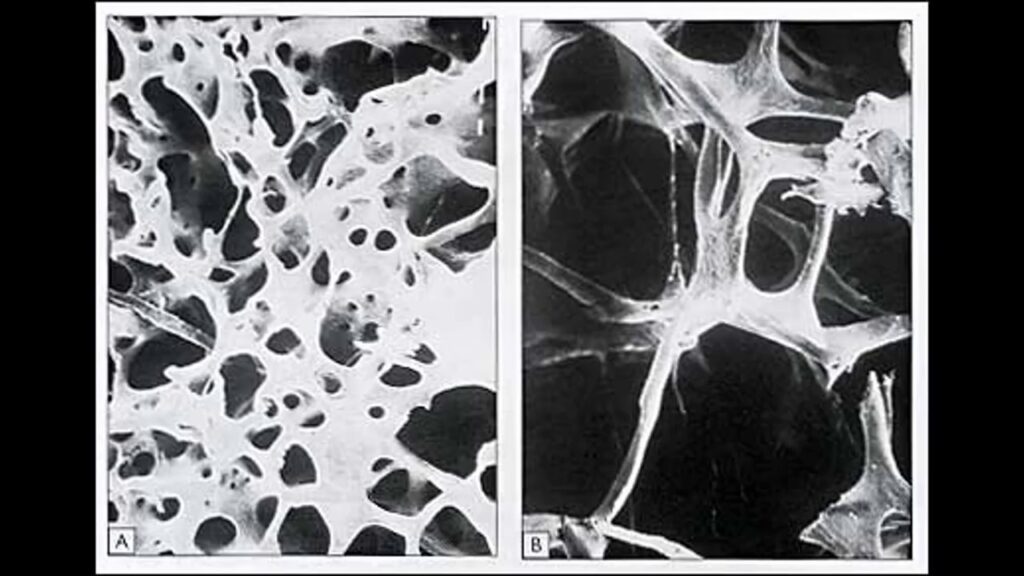
Bone matrix has been shown to be thinned in osteoporosis. While bisphosphonate treatment increases matrix formation and structure early in their use, they have been associated with causing matrix degrading over time. This is thought to cause brittle bone which is seen in transverse femur fractures with the use of these drugs. The image shows healthy bone matrix on the left and osteoporotic matrix in the right.
Studies using collagen supplements have largely not shown a strong beneficial effect in increasing bone matrix and structure. This, however, does not imply that supplementing with collagen is not important and helpful in osteoporosis. The catch is that not all collagen is the same.
All tissue has some type of collagen matrix that hold it together and imparts strength to that tissue. The collagen matrix in bone is a very specific weight of collagen peptides. Collagen fibers come in a variety of sizes and that found in bone is relatively fine. Most collagen peptides have a molecular weight of 300 kDa. That in the walls of the white blood cell neutrophils is 75 kDa. Most of the matrix in bone is only 5 kDa so a general collagen supplement supplies very little of it. Fortunately, a bone specific collagen is available, FORTIBONE® supplying 5 kDa peptides suited to bone matrix.
A study supplying 5 gm daily of this specific collagen for 12 months resulted in an increase in bone density an average 3.0% in the spine and 6.7% in the femoral neck, while scores in the placebo group declined further by 1.3% and 1.0% respectively. (2) For a reference point, bisphosphonate treatment results in a 5-7% increase in bone mineral density after 3 years of use.
An observation with herbal treatments such as what would be used for inflammation is that combining multiple herbs often generates an effect that is greater than simply adding up what each will do. The synergy appears to be greater than the sum of the parts. This is likely also true regarding putting bone matrix specific collagen together with the other steps we have outlined including:
- Quieting inflammatory driven osteoclast (bone removers) activity
- Stimulating “homing” of stem cells to bone with bone morphogenic protein (BMPs) supplementation
- Enhancing the release of BMPs in the diseased bone with low level laser
- Enhancing bone marrow release of stem cells for migration with low level laser
- Supplementation of urolithin A to restore function in older osteoblasts (bone builders)
The final blog in this series will review putting this all together in an effective treatment program now that we have discussed the important subject of restoring and maintaining bone matrix.
- Haworth AE, Webb J. SKELETAL COMPLICATIONS OF BIOSPHOSPHONATE USE: WHAT THE RADIOLOGIST SHOULD KNOW. Br J Radiol, 2012; 85(1018):1333–1342.
- König et al. SPECIFIC COLLAGEN PEPTIDES IMPROVE BONE MINERAL DENSITY AND BONE MARKERS IN POSTMENOPAUSAL WOMEN-A RANDOMIZED CONTROLLED STUDY. Nutrients 2018, 10(1), 97.
- Adams et al. POSTMENOPAUSAL OSTEOPOROSIS. TREATMENT WITH CALCITONIN AND A DIET RICH IN COLLAGEN PROTEINS. Cas Lek Cesk,1996 Jan 31;135(3):74-8.