Autoimmunity
December 1, 2022
One of a Few Common Chronic Diseases That We Are Now More Likely to Face
Advances in research have helped the U.S. enjoy decreasing rates of several chronic diseases over the past 3 decades. Autoimmune disease has been a notable exception to this trend increasing rather dramatically. This trend has been broad with sharp increases in all autoimmune diseases of which there are over 100 affecting virtually all areas of the body.
The immune system in a healthy, well-functioning state has the ability to differentiate friend from foe. Friend refers to our own tissue, food particles and good microbes such as in a healthy gut microbiome. Foe represents harmful things in our environment that we need protection from such as viruses and pathogenic bacteria. It is easy to appreciate this need to protect from foe being in the 3rd year of the COVID-19 pandemic.
Autoimmunity is basically a situation where the immune system loses its ability to tell friend from foe, or us from them, attacking our own tissues with inflammation and destructive antibodies. The emphasis in treatment has concentrated on the use of immune suppressing drugs. While this can diminish the attack and damage to “self”, it increases the risk of attack and damage from two other processes that the immune system is responsible for, eliminating pathologic microbes such as dangerous viruses and cells that have damaged/mutated DNA – cancer cells.
Most of the autoimmune diseases have been associated with genetic variations that weaken the ability of the immune system to distinguish pathogens from self-tissue. The common genetic variations are in genes in the HLA system. This system is like a chaperone that accompanies pieces of pathogens and other molecules when they are presented to the antibody producing immune system helping it tell what is appropriate to attack. Variant HLAs do this job poorly.
Genetics; however, are far from the whole story. Only about one-third of those who develop autoimmune disease have genetic variations that contribute to the disease development. Not everyone who has a specific genetic variation that increases risk will develop disease, and the majority who do develop autoimmune disease do not have these genetic risks factors.
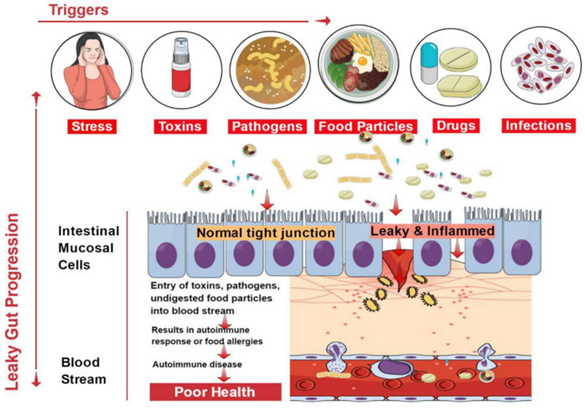
The other two-thirds of risk come from our environment. More recently extensive work is being done examining the relationship between the environmental factors and disease risk. This very broad area of risk is termed the “exposome”, or what we are exposed to that triggers the disease. It may involve chemicals, foods, and many other factors that confuse the immune system causing it to react to self-tissue as if it is foreign and dangerous.
An example of a food triggered autoimmune disease is celiac disease which is known to be caused by dietary exposure to gluten peptides. Different food peptides may have “sequence similarity” to proteins in our own tissue. In celiac disease different peptide pieces of gluten have similar peptide sequence as an enzyme in the small intestinal lining called tissue transglutaminase (tTG). If the immune system reacts to gluten producing antibodies against it, it may begin to misrecognize tTG as gluten attacking it destroying the lining of the small intestine.
Different food peptides may also share close sequence similarity causing an immune reaction against one to spread causing reaction to a second food. This is shown in the above image showing similarity between gluten and casein, a peptide in dairy. This is why many people who react to gluten will also react to dairy.
Chemicals, which are now prolific in our food, air, water, and virtually everything else we come in contact with trigger autoimmunity by other mechanisms which primarily alter the appearance of our own tissue proteins making them now look foreign/foe to the immune system triggering attack. Some chemicals do so by direct damage to our tissue proteins while others attach to these proteins making them look foreign.
Although work environments can be a source of concerning chemical exposure, the majority of these exposures come from everyday products that are commonly used such as food and personal care products (e.g., lotion, toothpaste, body wash, shampoo, deodorant, and many other products that people use daily.) On average, women use 12 personal care products a day, exposing themselves to 168 chemical ingredients. Over 80,000 chemicals are approved for use in our food supply while many remain inadequately tested for long term safety.
This focus on the relationship of the exposome and triggering of autoimmunity has expanded to correcting exposures and the ability to put these diseases into remission. The results are encouraging as we will explore in this series of blog posts. Using this information in prevention is ideal, but it is also helpful in treatment if disease is already present.