
Autoimmunity and Leaky Gut
December 8, 2022
The first line of defense in the body against invaders that can abnormally activate the immune system are our physical barriers such as the skin and intestinal barrier. The intestinal barrier is especially important for multiple reasons:
- It is the body’s largest barrier between the inside and outside worlds.
- It is exposed to a broad amount of potential activators of immune reactions including the gut microbiota, food peptides and environmental chemicals.
- It has the unique responsibility of allowing needed factors such as nutrients to pass but at the same time excluding passage to potentially harmful factors such as microbes.
If this barrier is “breached” the body is flooded with factors that activate inflammation and antibody production to fight them. If this is chronic and substantial, the risk of the immune reaction against the factors activating the immune reaction can cause the reaction to spread to our own tissues which appear similar – the process of autoimmunity.
The gut barrier is only a single epithelial cell thick separating the immune layer from the contents of the gut including microbes, foods, chemicals, and other contents. At first it would seem that a single cell barrier is not the best design, but it allows the passage of nutrients and needed food molecules in by passage through these cells. The day-to-day job of sorting friend from foe in the gut is dependent on the integrity of the gut barrier.
The science into the role of a dysfunctioning or “leaky gut” in autoimmune disease has found it to be an important part. (1) A recent review of the research in this area concluded, “An association of autoimmune diseases and leaky gut has emerged as a critical situation wherein the leakage of pathogens into the body system results in autoimmunity.”
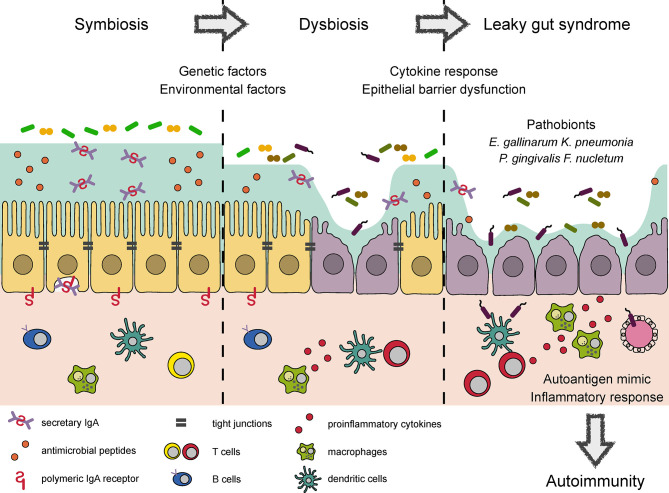
The gut epithelial cells are linked together by “tight junctions” to prevent the free passage of gut contents into the immune layer. These junctions are shown between the cells in the left side of the diagram. The tight junctions function as a gate allowing some things to pass and others to not pass. When the gate gets damaged as shown on the right side of the diagram, microbes, poorly digested food molecules and chemicals are free to pass into the immune layer triggering reaction.
The cell barrier has another layer of protection with mucin shown as the green area in the diagram. A healthy mucin layer helps keep the gut contents from directly accessing the cell layer. Unfortunately, many things can erode the mucin layer such as the use of anti-inflammatory drugs, while others such as stress inhibit the replenishment of mucin.
Different factors breakdown the gut tight junctions allowing the gut contents into the immune layer triggering inflammation and antibody production. This was first discovered looking for the source of the sustained diarrhea associated with cholera infection. (2) The toxin produced by the cholera bacteria causes the tight junction proteins, zonulin and occludin to breakdown opening the gate allowing water and chloride to flush into the gut. The purpose is thought to try to flush out the bacteria from the gut.
Subsequently, it has been shown that other factors such as gluten cause the same opening of the gut tight junctions increasing immune stress. (3) This tight junction breakdown and immune activation eventually causes antibodies to a section of gluten, alpha gliadin, to cross react with a tissue enzyme, tissue transglutaminase (tTG), destroying the gut lining. This cross reaction is a process where an antibody against a food peptide may also attack molecules of our own tissue that look similar. Other food peptides such as beta casein in dairy may trigger cross reaction with different body tissues.
In the next several blogs we will explore the many factors that cause leaky gut and increase the risk of triggering autoimmune disease. These include:
- Dysbiosis, or a shift in the normal microbiome to a less healthy composition.
- Food sensitivities or immune reactions against food molecules.
- Food additives such as emulsifiers.
- Dietary chemicals such as glyphosate.
- Stress
- Paray et al. LEAKY GUT AND AUTOIMMUNITY: AN INTRICATE BALANCE IN INDIVIDUALS HEALTH AND THE DISEASED STATE. Int. J. Mol. Sci, 2020;21:9770.
- Fasano et al. THE ENTEROTOXIC EFFECT OF ZONULA OCCLUDENS TOXIN (ZOT) ON RABBIT SMALL INTESTINE INVOLVES THE PARACELLULAR PATHWAY. Gastroenterology, 1997; 112: 839-846.
- Fasano et al. ZONULIN, A NEWLY DISCOVERED MODULATOR OF INTESTINAL PERMEABILITY, AND ITS EXPRSSION IN COELIAC DISEASE. The Lancet, 2000;355:1518-1519.