
Long-Haul COVID-19: What causes it and how to treat it
January 20, 2022
Long COVID-19 affects about 20% of those who develop the infection. Currently in the United States there have been over 62 million documented infections which would put the number of persons with long COVID-19 symptoms at greater than 12.4 million. Of equal concern is the fact that the number of infections now occurring is greater than 200,000 daily which will continue to expand the long-COVID-19 population.
Generally, long COVID-19 is the persistence of symptoms such as fatigue, shortness of breath, joint pain, loss of taste or smell and anxiety for 4 or more months after testing suggests the infection is no longer present. The presentation varies widely from person to person, but the relationship to previous infection is universal.
Many researchers suggest that long-haul COVID-19 is a variant of ME/CSF or myalgic encephalomyelitis/chronic fatigue syndrome which is well known to be triggered by viral infection. The dominant feature of CFS is excessive fatigue, particularly with exercise and is not resolved by rest.
Several research groups have looked at markers of what is different between those who fully recover from COVID-19 and those who have persisting symptoms. The most notable finding is that the first immune response to any infection, inflammation, does not appear to resolve or turn off in those with persistent symptoms.(1) While little data is available about the levels of inflammation in patients before they become infected, it is likely that they have higher levels of inflammation before the infection, the infection elevates it significantly more and the immune system is not turning it back off as it should after any immune challenge.
Support for this concept comes from a comparison of symptoms during an acute infection such as a bad cold or the flu. Fatigue and aching are common features during the infection, but they typically disappear as the infection resolves. These symptoms are not from the infection directly but rather are from our own immune response. Once the inflammatory response activates to begin to kill the infection and signal the acquired immune system to produce antibodies, the inflammation should begin to reduce.
The process of resolution of inflammation is not passive, and it requires an active shift in immune response to the “resolution stage”. Several things must be in order for immune resolution and it is likely that these factors are not balanced going into the viral infection. Factors that are known to affect resolution are many including:
- Diet
- Anxiety
- Cell omega fatty acid levels
- Body composition
- Co-morbidities
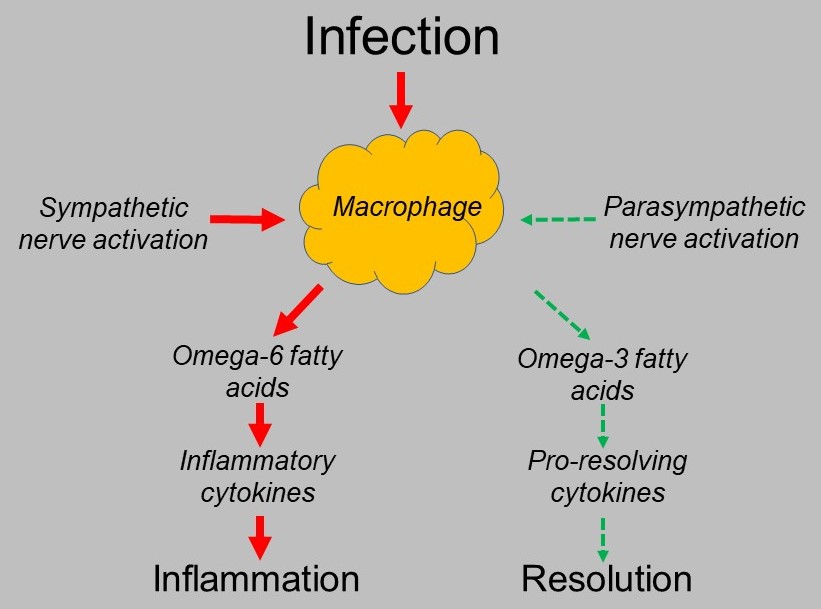
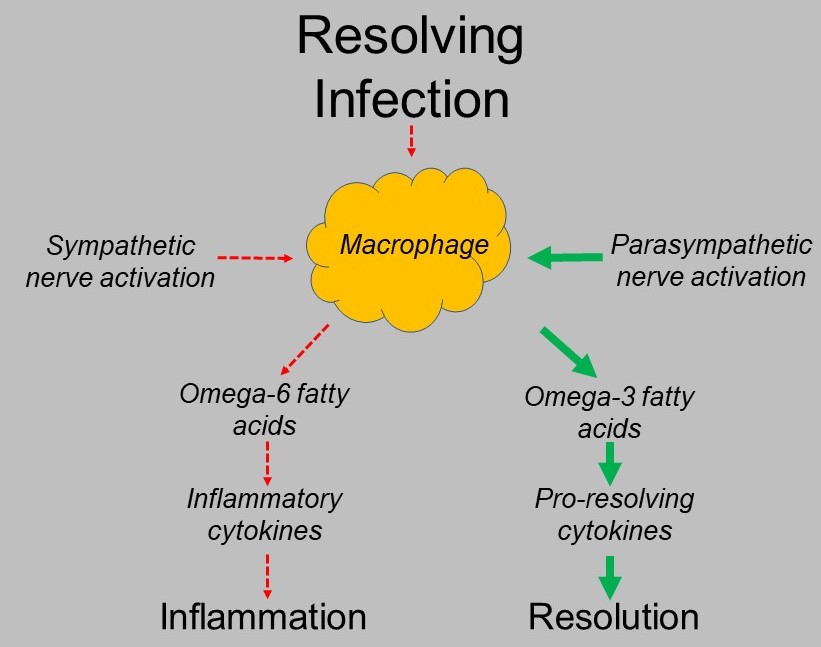
The resolution of inflammation is an active process. Inflammatory initiation is done by innate immune cells called macrophages. They produce chemicals called cytokines which activate inflammation. These cytokines are made from omega-6 fatty acids such as arachidonic acid which is very rich in grain, the vegetable oils used in processed foods and in meat/eggs/dairy from grain fed animals. When it is appropriate to stop or resolve inflammation, the macrophages switch their behavior and extract omega-3 fatty acids from their cell membranes which they convert to pro-resolving mediators.
This ability to turn on inflammation when appropriate and resolve it when appropriate is dependent on the proper balance of omega-6 to omega-3 fatty acids in the macrophage cell membranes. This balance is dependent on the omega-6 to omega-3 fatty acid balance of the diet which is very skewed in the western dietary pattern. Ideally the omega-6 to omega-3 ration should be between 1:1 and 2:1. The ratio of the typical American diet is 16:1 or very pro-inflammatory.
Other dietary factors that cause too much inflammatory signaling are high sugar consumption and high saturated fat consumption. An accurate summary of the typical American diet is one with too much sugar, a very high omega-6 to omega-3 ratio and one that is high in saturated fat.
Anxiety is a state where the autonomic nervous system that controls all unconscious function has too much sympathetic, or “fight or flight” activation and too low parasympathetic function which moves our internal state to “rest, digest and repair”. The signal that tells macrophages to take omega-6 fatty acids from the cell membrane to produce inflammatory cytokines is that of sympathetic activation while parasympathetic activation triggers the resolution phase. Stressed and anxious is pro-inflammatory. Low parasympathetic activity causes failure of signaling to the resolution phase.
Most do not think of body composition when considering their inflammation. It is perhaps one of the more important factors. The factor that most correlated with the risk of severe COVID-19 was comorbidities. Medically, this simply means what chronic diseases exist in a patient. Diabetes, hypertension, heart disease and several other chronic diseases highly correlate with the risk of severe COVID-19 infection and outcome including long COVID-19 risk. What these diseases have in common is that excessive central body fat predisposes to all of them. Why? Body fat in the center of the body (belly and hips) produces inflammation. Obesity has proven to be the most predictive indicator of a poor outcome with COVID-19 infection.
Just as all of the above factors drive inflammation, they are thought to be the drivers of long COVID-19. Appropriate intervention to resolve long COVID-19 involves:
- Measure the level of inflammatory activation. Blood markers such as CRP and sedimentation rate help to measure this.
- Measure cell omega-6 and omega-3 fatty acid levels.
- Begin high dose omega-3 fatty acid supplementation.
- Begin herbal suppression of inflammatory activation with curcumin, resveratrol and other NFκB inhibitors. NFκB is the transcription factors that activate inflammatory cytokine production. This is a different mechanism of trying to suppress inflammatory signaling with NSAIDs such as ibuprofen which is associated with a number of adverse effects in large quantities.
- Reactivate mitochondrial energy processing. Mitochondria are the energy producing organelles within cells that produce ATP which is cell energy. This process is disrupted with chronic inflammation and is the likely source of the chronic fatigue. This is done with high amounts of nutrients involved in mitochondrial processing such as riboflavin, CoQ10, thiamine, acetyl-L-carnitine, niacin and magnesium. One of the other mechanisms which impair mitochondrial energy production is the build-up of senescent mitochondria that no longer work. These must be removed by a process called autophagy which can be stimulated by high doses of flavonoid supplementation.
- Removing other factors that cause chronic inflammatory activation such as food sensitivities or dysbiosis of the gut microbiome. Being “pre-inflamed” prior to COVID-19 infection is likely a major factor in the differences in long-term outcome from one person to the next.
- For the more specific symptoms such a neuropathy, a laser therapy program will help heal and restore function in injured nerves. Both the loss of taste and smell are forms of neuropathy with damage to the sensory nerves that integrate taste and smell. Laser therapy has recently been shown to resolve this dysfunction in the majority of subjects.(2)
For the 12.4 million plus who have long-COVID-19 and for the many more who will likely develop it, there is a way out of it. It is important to figure out the pieces involved in each case and putting together the appropriate program to aid resolution. It may well make the difference in getting a life back.
- Doykov et al. The Long Tail of COVID-19 – The Detection of a Prolonged Inflammatory Response After SARS-CoV-2 Infection in Asymptomatic and Mildly Affected Patients. F1000 Research, 2021;9:1349.
- Compos et al. PBA Brazilian multicenter pilot case series on the efficacy of photobiomodulation therapy for COVID-19-related taste dysfunction. Photodiagnosis and Photodynamic Therapy, 2021.