
The Many Faces of Food Sensitivities
January 14, 2021
IBS – Part 2
Food sensitivities and food allergies are often confused. Persons suspected of having a food sensitivity often report, “I was tested for that and nothing was found”. More in-depth discussion reveals that testing was done with skin testing, a method of testing that examines allergies rather than sensitivities.
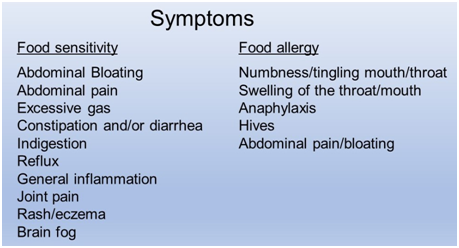
Allergies are caused by a fast reacting antibody called IgE. Symptoms typically occur directly after eating the specific food and include features such as swelling or tingling of the mouth and/or throat, hives, swelling, and occasionally, relatively rapid onset GI symptoms. Sensitivities in contrast, are hallmarked by delayed, gradual onset of symptoms such as abdominal pain, bloating, indigestion, reflux and constipation and/or diarrhea. They may also be associated with many other non-GI symptoms such as joint pain, skin conditions such as eczema, thyroid disorders, brain fog and other brain/mental symptoms.
While food allergies are relatively rare occurring in less than 5% of the population, food sensitivities are more commonly thought to affect as much as 15% or more. This percentage may be significantly under-estimated given the relatively poor understanding of food sensitivities in the broader health care community. They have only been more broadly studied over the past decade.
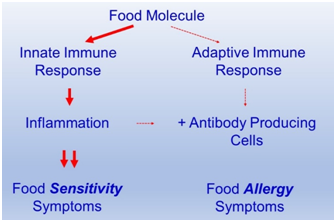
The recognition of food sensitivities has been hampered by the lack of a diagnostic biomarker in many cases. A biomarker is something that can be measured confirming a specific disorder such as IgE antibodies seen in food allergies. Sensitivities are thought to be caused by inflammatory activation by the innate immune system which is difficult to measure with lab tests. Eventually, the innate immune response may trigger activation of the acquired immune system, the side that makes antibodies such as IgG. It is thought that food sensitivity reactions often do not trigger this acquired immune response and thus no biomarker.
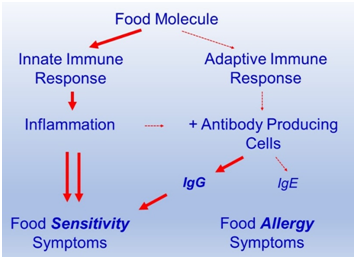
The figure below shows the addition of the slow reacting antibody IgG in some cases of food sensitivity. In these cases the problem can be confirmed with IgG antibody testing. However, a substantial portion of food sensitivity reactions are restricted to the innate immune response shown in the top diagram only causing symptoms mediated by inflammatory signaling which is more difficult to measure.
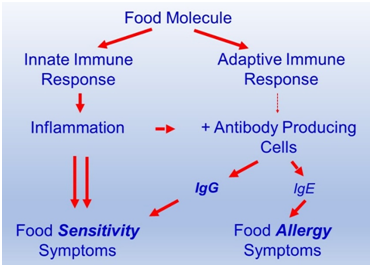
Food allergy, in contrast, is an aggressive, quick response caused by the adaptive immune system that is responsible for making antibodies which mediate the majority of the response with IgE. Food allergies are demonstrated by skin testing where a small amount of the food molecule is injected into the skin and grading the degree of the wheal or swelling and redness. Blood tests to IgE antibodies can also be done but each form of testing can give inaccurate results.
In most cases food sensitivity can be screened with meridian response testing called a Biomeridian test. The test measures meridian point galvanic responses which in a healthy functioning system remain in a desired range. The electromagnetic signal of different foods can be introduced and the meridian point remeasured.
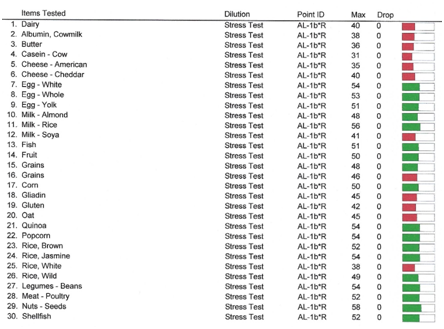
For non-reactive foods, the point is unaffected. When there is a strong negative response to the food, the point drops considerably. This testing is thought to be about 70% sensitive and accurate. It leads to a food or group of foods to avoid. Improvement with strict avoidance of the suspected food over 3-4 weeks confirms the sensitivity.
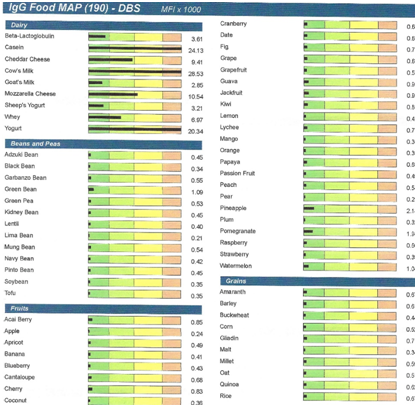
In cases where meridian response testing does not yield specific answers, blood IgG antibody testing can be done. In exceptionally challenging cases both types of testing can be used to add more clarity. In each case, the initial impression derived from the testing is confirmed by improvement in symptoms with a 3-4 week strict avoidance of the positive foods.
A problem that often complicates food sensitivities is gut barrier dysfunction or “leaky gut”. The inflammation induced by the food reaction triggers the release of the enzyme zonulin by the lining cells of the small intestine. This enzyme disrupts the junctions between the epithelial cells that line the intestinal lumen preventing other food molecules and bacterial components from reaching the immune layer of the intestinal wall. This allows many food particles to reach this immune activating tissue triggering extensive food reactions. The hallmark of leaky gut is the broad reactivity to many foods. Primary sensitivity reactions are typically limited to 1-3 foods and positive testing for extensive foods is unknown in the absence of leaky gut. In these cases the most common reactive foods which include a dairy peptide casein, gluten and nightshades are removed from the diet and reparative supplementation for the gut barrier including L-glutamine, glucosamine, MSM with coating substances such as aloe vera and okra is used. Once the gut barrier heals, many foods can be reintroduced without symptoms as long as the primary reactive 1-3 foods are avoided. One of the great challenges in managing food sensitivities is that the primary reactive foods cannot be reintroduced once symptoms are resolved for a significant period of time. One of the traits of the immune system that we appreciate is that it exhibits memory. Once we have reacted to a challenge such as an infection, we have memory cells that have been programmed to remember molecules on that organism called antigens. These memory cells react quickly if exposed in the future preventing reinfection. Once immune cells react to a food antigen, they exhibit immune memory and react quickly again if it is reintroduced