The Omega-3 Fatty Acid DHA Offers Protection Against Alzheimer’s Disease
July 12, 2022
Omega-3 fatty acids (FAs) are essential fatty acids. This means that the body needs them for different functions, and they must be consumed as the body cannot make them from other sources. Systems that are particularly dependent upon the availability of omega-3 FAs are the immune system, the cardiovascular system and the brain.
There are 3 primary omega-3 FAS, EPA, DHA, and DPA. Each have distinct and overlapping functions. More recent research has looked at these individually and is helping to define their roles in disease prevention. DHA has perhaps been the lessor understood, but it is now being appreciated for its importance in immune function and brain function. Its immune function is to supply the production of a group of fatty acids which resolve inflammation and stimulate tissue healing.
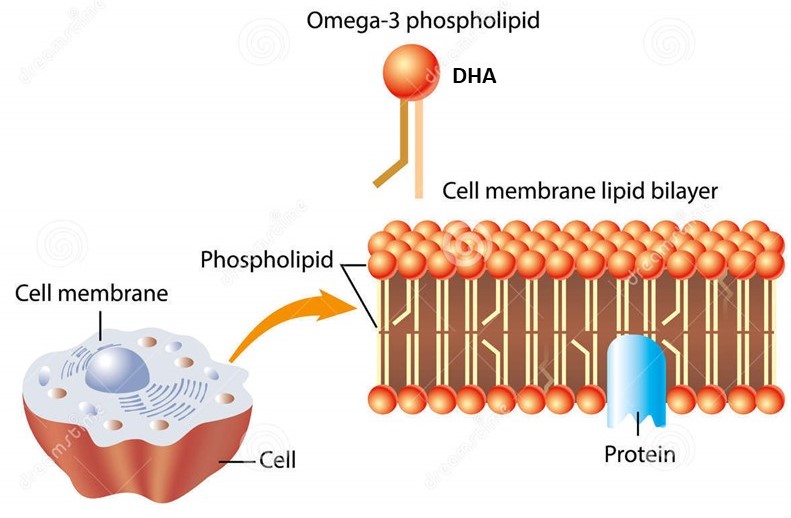
The Omega-3 FAs are also an integral part of cell membranes including neurons, the nerve cells in the brain and peripheral nervous system. The brain seems to be especially dependent on the cell levels of DHA. A new study made this point well. The study looked at red blood cell membrane DHA levels and their relationship to the risk of developing Alzheimer’s disease.
This study was part of the long running Framingham study. A testament to how long this study has been going on, it used offspring of the original Framingham study participants who were >65 years of age. The DHA content of their red blood cells was used to reflect brain cell levels. Red blood cells are a common “surrogate” marker of the levels in all of our cell membranes, and they are easy to obtain with a finger prick sample.
After 7 years of observation 131 cases of Alzheimer’s Disease had developed. Those who were in the highest quintile (top 20%) of DHA levels had a 49% reduced incidence of Alzheimer’s Disease compared to those in the lowest quintile. The researchers stated that “the increase in RBC DHA from Q1 to Q5 was predicted to provide an estimated 4.7 additional years of life free of AD.”
Another observation was that this reduced risk was greatest in those who were carriers of the APO E4 gene which is the major genetic risk factor for the disease. The genetic risk is not an absolute predictor of the disease. It rather appears to predict that those persons with APO E4 must be that much more precise with their lifestyle to prevent it.
How much of the preventative effect DHA imparts for neurodegenerative disease relates to how it supports the immune functions and how much from direct brain cell membrane function is unknown. We just know at this point that higher cell levels of DHA reduce disease risk.
As stated above, DHA must come from diet. All omega-3 FAs originate in the plant world from a precursor, alpha linolenic acid (ALA). ALA is rich in green plants, flax seed, chia seed and other foods such as healthy nuts. ALA must be enzymatically converted to the active omega-3s including DHA. Several things must be in order for that to happen including:
- Adequate consumption of high ALA foods
- Sufficient enzymatic conversion of ALA to active omega-3s
- Adequate consumption of animal fats containing omega-3s
The U.S. diet simply fails the first in this list. Many people have gene variants and make low levels of the enzymes that convert ALA to active omega-3s. Many of the animal sources that humans had obtained omega-3s from have had their content of those fatty acids greatly reduced based on what those animals are now fed. A few hundred years ago it was primary grasses which were a rich source of ALA. Now they are fed predominantly feeds such as corn and soybeans which are very poor sources of ALA. The result is meat/milk/eggs low in omega-3 FAs.
The densest omega-3 rich animal foods are fish. The ALA source in the fish world comes from green algae which krill consume. They are eaten by a small fish who becomes food for the bigger fish. While fish oils are the densest source of omega-3s, they can also accumulate mercury and PCBs so it is important to use an oil that is certified free of these contaminants.
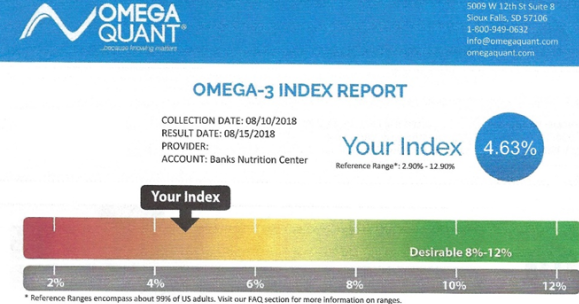
The last questions are how much do we need and how do we know when we have enough? The goal is to have the red blood cell membrane omega-3 content be >8%. As it is variable how much an individual must consume to reach 8%, having a red blood cell omega-3 level test is important. In the example shown the omega-3 content is low at 4.63%. Generally with this level, supplementation with 1500-2000 mgs of omega-3s would be given and the test re-done in 4 months.
Many fish oils contain high amounts of EPA but much lower amounts of DHA. It is important to take an oil balanced in the amounts of DHA and EPA. The level of supplementation is then adjusted up or down according to the follow-up test.
Our food has changed and these changes are being found to highly correlate with disease risk. Lorin Cordain, PhD who is perhaps one of the top scientists in how our diets have changed and disease risks estimates that our paleolithic ancestors consumed 4000-5000 mgs of omega-3 FAs daily. The U.S. average is now about 500 mgs or a 10 fold reduction. Fortunately, we are understanding more about these relationships and how to compensate them.
Sala-Vila et al. RED BLOOD CELL DHA IS INVERSELY ASSOCIATED WITH RISK OF INCIDENT ALZHEIMER’S DISEASE AND ALL-CAUSE DEMENTIA: FRAMINGHAM OFFSPRING STUDY. Nutrients, 2022;14:2408.