Why Celiac Disease is Increasing
Celiac disease is an autoimmune disease in which an immune antibody reaction to gluten begins to cause cross reaction against the lining of the small intestine. It is associated with intestinal symptoms such as abdominal pain, bloating and diarrhea as well as many symptoms outside of the digestive tract such as fatigue, anemia, osteoporosis, joint pain and many more.
Cross reactivity is where the immune system sees a segment of a peptide in gluten and then begins to recognize similar segments of peptides in our own tissue. In celiac disease, the immune cells reacting to a peptide portion of gluten, recognize a similar peptide sequence in an enzyme in the intestinal lining called tissue transglutaminase (tTG) and make antibodies which attack the intestinal lining. Over time, more tissues can become involved in this cross reactivity. An example is immune injury to an important area of the brain in balance and coordination called the cerebellum. This causes a significant balance disorder called gluten ataxia.
A consistent observation over the last 3 decades has been the prevalence or the percentage of the population with celiac disease as well as other gluten related disorders has been increasing.(1) This naturally has led to increased research as to “why”.
The answer seems to involve several factors. These include:
- Grain production is highly hybridized to only a few strains of wheat. This was to increase protein content in response to world hunger and protein calorie malnutrition. The main wheat protein – gluten.
- Bread is now raised chemically in 1 hour rather than through a long fermentation process by yeast and bacteria. The yeast and bacterial enzymes would breakdown much of the gluten during fermentation.
- Grain consumption in western nations has increased over the past 100 years.
Yet another cause of the increase in celiac disease and other gluten related disorders over the past 3 decades has been an increased exposure to food additives, pesticide residues and other chemicals. These chemicals have been shown to cause breakdown of the gut barrier, a problem commonly called leaky gut. The gut barrier is made up of epithelial cell, but it is only 1 cell thick. Directly under this barrier is the immune layer where inflammation and activation of antibody producing cells can be triggered.
Generally inflammatory activating bacteria and larger, poorly digested food molecules called peptides cannot cross this barrier into the immune layer as they can activate these immune responses. Small molecules called tight junction protein hold these epithelial cells together preventing leaky gut. Some food molecules like gluten and some environmental chemicals cause the release of an enzyme called zonulin. Zonulin’s job – it causes breakdown of the tight junctions allowing leaky gut.
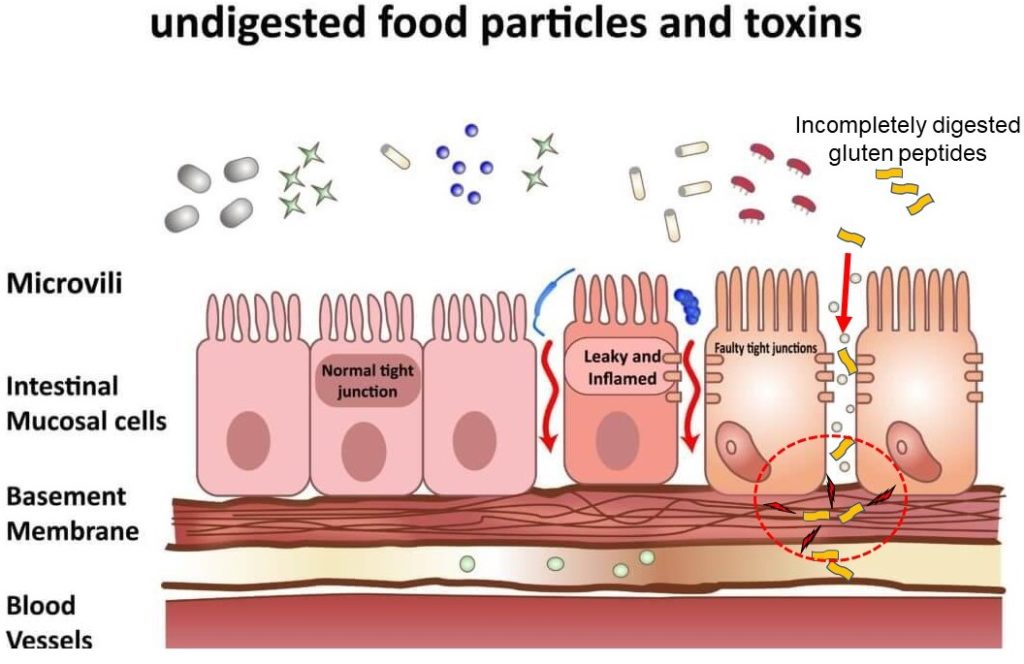
In a new study researchers looked at the relationship between chemical exposures and celiac disease.(2) The link was thought to be related to certain chemicals triggering zonulin inducing leaky gut allowing gluten peptides into the immune layer. In the study, those with higher serum levels of a common chemical class in pesticides, dichlorodiphenyldichlorethylenes (DDEs), had a doubling of the incidence of celiac disease compared to those with low levels.
There were gender differences in the susceptibility of different chemicals and the triggering of zonulin and celiac disease. Females with high serum levels of perflouoroalkyls, or PFAs, chemicals from non-stick surfaces such as Teflon, had an 8-fold increase rate of celiac disease. Males with higher serum levels of polybrominated diphenyl ethers, or PBDEs found in flame retardants in everything from carpet to furniture, had a doubling of the risk of celiac disease compared to those with low levels.
The protection against these chemical-triggered gluten related disorders requires a combined approach; eating less gluten, eating organic to avoid pesticide residues, avoiding food additives, and supporting good detoxification. A yearly detoxification program is a more important consideration than ever before. In some individuals, gluten by itself will trigger zonulin release causing a leaky gut which allows the incompletely digested peptide into the immune layer. For these individuals, avoiding gluten and cross-reactive food peptides such as in dairy are the solution.
When I was in grad school we had to read a book “Anything Can Cause Anything”. I thought the book was an exaggeration. Every year I practice it becomes more prophetic. When I retire I plan to write my book on what all these years have taught me, “Everything Can Cause Something”!
King et al. INCIDENCE OF CELIAC DISEASE IS INCREASING OVER TIME: A SYSTEMATIC REVIEW AND META-ANALYSIS. Am J Gastroenterol 2020;00:1–19.
Gaylord et al. PERSISTENT ORGANIC POLLUTANT EXPOSURE AND CELIAC DISEASE: A PILOT STUDY. Environmental Research, 2020;186:109439.