
Infection, Vaccination, and Autoimmunity
April 13, 2023
I unconsciously held this information in our autoimmunity blog discussions till last. This was the result of the highly emotionally charged discussion regarding the SARS-CoV2 pandemic and vaccination in the back of my mind. A fair analysis supports the point that each camp makes:
- Yes, vaccination has been shown to trigger autoimmunity.
- Yes, infection is a well-known trigger of autoimmunity.
When all the data is examined, both points are true. This suggests that each decision needs to be evaluated in light of all of the data on both sides as well as the individual factors that create their unique individual risk in either situation.
An example of infection triggered autoimmunity include SARS-CoV-2 infection. A study of almost 4 million subjects between the 2-year period of January, 2020 and December, 2021 found that those infected had increased rates of new onset of several autoimmune diseases ranging from a 78% rate of inflammatory bowel disease to 200% increased rates of lupus, rheumatoid arthritis, and ankylosing spondylitis.(1)
Type 1 autoimmune diabetes has been known to be associated with an enterovirus, coxsackie B4 virus which is a common digestive tract viral infection. Examination of 24 studies looking at the association found that infection with this virus increased the risk of type 1 diabetes between 5.5 to 17.4 fold.
Similar relationship between rotavirus, another common digestive viral infection in children, and type 1 diabetes has been shown. Herpes viruses such as Epstein–Barr virus have been associated with triggering type 1 diabetes as have respiratory viruses such as Influenza A Virus. Several other autoimmune diseases such as multiple sclerosis have also been shown to be associated with these viral infections.
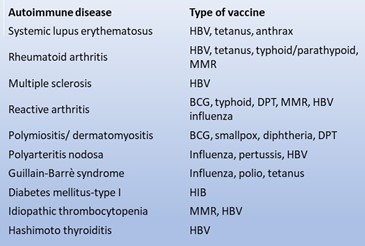
Interestingly, similar studies associated vaccination with autoimmune risk.(2) This risk is spread across several autoimmune diseases and associated with several different vaccinations. Guillain–Barré syndrome (GBS) which is an autoimmune disease which affects peripheral nerves causing muscle weakness, occurs following several vaccinations. In 1976 vaccination against the H1N1 virus caused over 500 cases of GBS including 25 resulting in death from 45 million vaccinations. The vaccination campaign was stopped as it was thought to be an excessive risk.
With the above findings, risking infection or risking prevention with a vaccine seems to be the literal “damned if you do and damned if you don’t” situation. There are factors that should be weighed for each individual in evaluating risk. These include:
- Immune status
- Prior infection or vaccination reactions
- Virulence of a particular infection
The above factors inter-relate. For example, with SARS CoV-2 infection appeared to be significantly more virulent than infections such as seasonal flu. As age generally is associated with declining immune function and greater immune risk, this virus had a dramatic age-related variation in death rates. Those 65-75 years of age had death rates from the infection of 3.5 times that of 18-29 year olds. Those >85 years had a risk of death 350 times greater than the 18-29 year olds. This would suggest that accepting the risk of vaccination would be more important in these older populations.
A better picture of risk happens looking at age/immune status and virulence of an infection together. Between 2020 and 2023 deaths associated with influenza were only 0.1% of all deaths in 18-29 year olds while deaths from SARS CoV-2 accounted for 3% of deaths in that age group. Not getting vaccinated in a healthy 18-29 year old may be an acceptable risk.
In contrast, while influenza accounted for only 0.2% of deaths in 65-74 year olds during those years, SARS CoV-2 accounted for 11.4% of deaths suggesting that more consideration of vaccination is warranted.
As autoimmune diseases often begin with milder fleeting symptoms, unusual, lingering symptoms following an infection or vaccination may suggest a transient autoimmune activation. Triggering that again is thought to increase the risk of disease progression. Any prior vaccine reaction suggesting a transient autoimmune reaction should suggest higher levels of caution.
I finish writing this blog with a feeling that the reader is left without black and white answers. That feeling would be accurate as we really do not have them and only have some shade of gray implications. Several analyses have suggested that the risk of triggering autoimmune disease is significantly higher from infection than it is from vaccination. Intense work is being done to sort all of this out with the hope that those at risk with either an infection or a vaccination can be identified and helping them pick the safest path for themselves.
So I end this as I started, hesitant. We like black and white answers, but in this case best we have is shades of gray.
- Chang et al. RISK OF AUTOIMMUNE DISEASS IN PATIENTS WITH COVID-19: A RETROSPECTIVE COHORT STUDY. eClinicalMedicine, 2023;56:101783.
- Vadala et al. VACCINATION AND AUTOIMMUNE DISEASES: IS PREVENTION OF ADVERSE HEALTH EFFECTS ON THE HORIZON? EPMA J. 2017 Sep; 8(3): 295–311.