Interesting New Information on Covid-19
November 2, 2021
As the Covid-19 pandemic lingers on well into year 2, the knowledge base concerning it is growing. This is largely the result of more study which requires greater numbers of persons and longer intervals of observation. While immunity was the burning question in 2020, how lasting immunity is, seems to be the question in 2021. An excellent study of over 1600 immunized health care providers has recently been reported. Those who chose not to be vaccinated as they have already been infected may be thinking, “no need to read this”, but it is also applicable to those situations.
The study tracked their antibody levels against the SARs-CoV-2 spike protein that the virus uses to attach and infect cells. Sequential measurements were done both in July, 2021 and October, 2021. As expected, antibody levels declined significantly over that interval. They also tracked antibody levels at follow-up and the risk of break-through or re-infections. There was a telling relationship. Those with the highest levels of antibodies at follow-up had no breakthrough infections, or 100% protection. Of those who had intermediate antibody levels 10% had breakthrough infections, or the group had 90% protection. The lowest antibody group only exhibited 12% protection suggesting that the antibody levels had regressed close to pre-vaccination levels.
The respective antibody levels for the 3 groups were <180 BAU/ml, 181-2190 BAU/ml, and >2190 BAU/ml. The BAU/ml is the number of binding antibody units per ml of blood. The specific test used was a quantitative antibody test, or a test not just for the presence but rather for the quantity of antibodies. These unit measures are specific for the SARS-CoV-2 Semi-quant Total Ab test from LabCorp. Different labs use different test methods, so the values may be slightly different.
The takeaways from this study are:
1 – The antibody response to the vaccination does not remain at a highly protective level indefinitely. This quantitative antibody test between 6-8 months after vaccination may be the ideal way to know if and when a booster may be needed.
2- Different people appear to develop different levels of antibodies in response to the same vaccine inferring more or less immunity. Different people appear to have differing time periods of the antibody response.
A related discussion is how do those who have had the infection and do not get vaccinated fair with the durability of antibody levels over time? That was not studied here so it is hard to answer that. The earlier study had indicated that infection did not produce as many long-lasting antibody producing cells suggesting that subsequent antibody protection would not be as durable. It will take a similar study looking at antibody levels over time in those who have been infected to make that judgment.
In either scenario, vaccinated or previously infected, it may be best to do a quantitative antibody test 6-8 months out to answer this question for a specific individual.
Dimeglio et al. Antibody titers and protection against a SARS-CoV-2 infection.J Infect. 2021 Sep 21;S0163-4453(21)00483-7. Online ahead of print
Another useful understanding that has come from newer research is about why different persons may have relatively quick resolution of the SARs-CoV-2 infection and others may develop severe disease possibly causing death. The key factor differentiating these outcomes is whether or not an individual develops “cytokine storm”.
Cytokines are immune signaling molecules that instruct immune cells to either produce inflammation (pro-inflammatory cytokines) or to resolve inflammation (resolving or anti-inflammatory cytokines). In the beginning of an infection inflammation is an important tool the immune system uses to attack the virus. However, the inflammation attacks our tissue as well. This can be tolerated for a moderate interval, but then it causes significant harm to us if not reversed. The most dangerous has been the acute respiratory distress that can often lead to lung failure and death.
After a reasonable interval of inflammation to control the infection, the immune cells that produced the inflammatory cytokines undergo “phenotypic shift” or a change in activity to stop producing inflammatory cytokines to anti-inflammatory cytokines called specialized pro-resolving mediators, or SPMs. To make these SPMs the cells take omega-3 fatty acids from their membrane and convert them into SPMs. This is why the omega-3 fatty acids are thought of as helping inflammation and healing. The production of these SPMs is dependent on adequate levels of omega-3 fatty acids in the cell membrane, a situation that often does not exist as they are typically inadequate in the western diet.
A recent study looked at SPM levels in healthy subjects, patients with severe COVID-19, and patients with mild recovering COVID-19. Compared to healthy subjects, patients recovering after only mild disease COVID-19 had higher circulating SPM levels. In other words, they had enough membrane omega-3 fatty acids to produce high levels of anti-inflammatory, pro-resolving cytokines. In contrast those who developed severe disease had abnormally low SPM levels.
The message here seems simple. Having healthy omega-3 fatty acid levels is protective against developing severe disease. The question then gets asked, how do we ensure we have adequate omega-3 levels? It is not linearly related to the level of dietary and supplemental omega-3 fatty acids consumed. There are multiple enzymes involved in getting them from diet into cell membranes, and these vary in efficiency from person to person. The best way to determine if adequate levels exist is to test cell membrane levels. This can be done with a simple finger prick blood test which looks at levels in red blood cells. They are simple to collect and are reflective of the levels in immune cells.
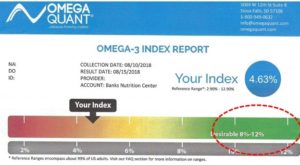
At least 8% of the cell membrane fatty acids ideally should be omega-3 fatty acids. The test shows an inadequate cell level of 4.63%. Typically, this person would be supplemented with about 2000 mgs/day of high grade fish oil which is a potent source of omega-3 fatty acids. The test should be redone in 4 months to ensure adequate levels have been achieved.
Beginning high dose omega-3 supplementation once infection has begun may help some, but it is a gradual process to incorporate these into the immune cell membranes so it is best done preventively. If concern about COVID-19 is not enough, chronic inflammation because of poor resolution is known to be an important part of almost every chronic disease from heart disease to cancer.
Koenis et al. Disrupted Resolution Mechanisms Favor Altered Phagocyte Responses in COVID-19. Circulation Research, 2021;129:e54–e7.
We had all hoped this pandemic would have been behind us early in 2021. Unfortunately, it is not and looks as if it is something we will manage with better understanding over time. Research in this area is occurring at a truly amazing rate. The result is better knowledge to get us safely through this.