The Stressed, Inflamed Loop of Depression
January 7, 2021
A Path Out of It with Drugless Treatment
Depression is a significant problem affecting 15% or 1 in 6 adults at some point in life. It is the leading cause of disability in developed nations. The stress of the pandemic has made things worse. A new study published in the Journal of the American Medical Association found that the rates of reported signs of depression increased 3-fold in the past year.(1) The trigger – stress.
How stress causes the brain to function in a pattern of depression has been heavily studied and the answer appears to be that stress causes inflammation. The inflammation in turn causes several maladaptive effects in the brain. Many experts explain that humans do not have a primary stress response but rather they have a danger response. Its purpose is to improve the odds of survival.
If we face danger, several body systems change their function often by inducing changes that if only active in the short term help survival without causing harm. One example is the increase in blood pressure. It delivers more blood to the muscles and brain to prepare for “fight or flight”. In the short term this helps and does little damage. If this reaction persists over the longer term, hypertension exists increasing the risk of heart disease, stroke, kidney disease and many more.
It seems that simply “stress” triggers many of the same “fight or flight” changes, but stress is more often ongoing than true danger causing these changes to actually be harmful. One such change is inducing the immune system to increase inflammation. The theory of this increase is that inflammation is part of the immune response to infection and to subsequent healing of injury. Fight or flight resulting in injury needs to be healed. However, longer term inflammation is injurious to almost all body systems including the brain.
The chemicals the immune system uses to increase inflammation are called cytokines. Extensive research has found elevated levels of inflammatory cytokines in depressed subjects compared to non-depressed controls. One of the ways inflammation alters brain function is by reducing levels of the mood regulating neurotransmitters thought to be a primary cause of depressive symptoms, serotonin.
Serotonin is made from the amino acid tryptophan, but under some conditions tryptophan can be alternatively converted to another neurotransmitter, quinolinic acid.
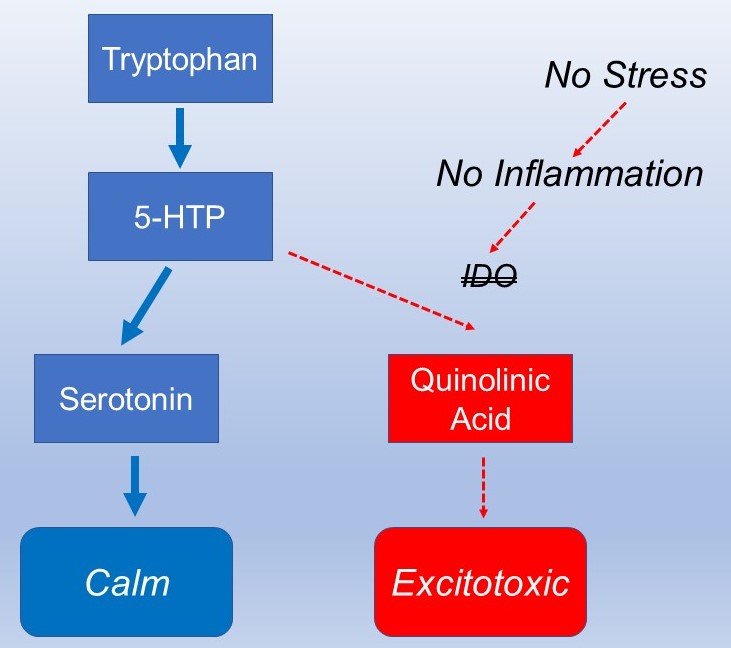
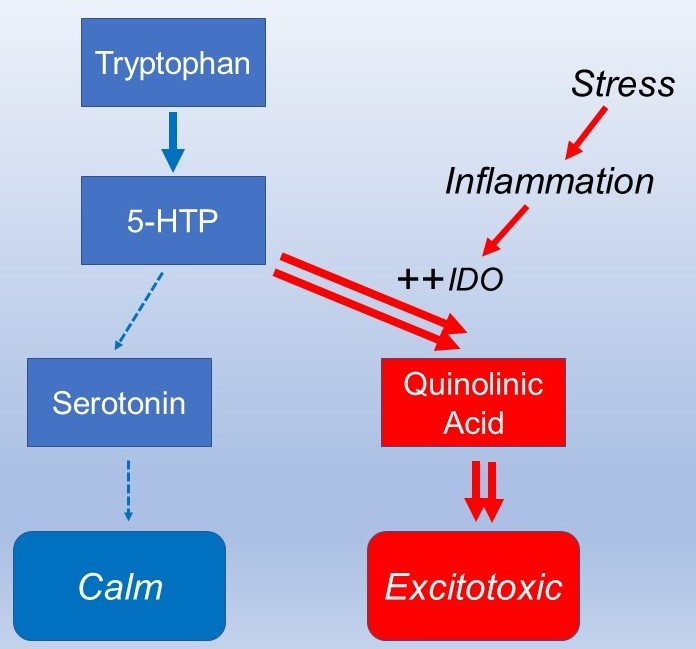
The brain then becomes low in the mood regulating serotonin but has higher levels of the excitotoxic quinolinic acid. The most understood condition where this switch occurs is during inflammation. While excitotoxicity can make the brain more alert to be better prepared for “fight or flight”, it is damaging if sustained over the longer term.
Interestingly, 30-40% of patients placed on drugs aimed at raising serotonin do not respond. This is because other factors in addition to low serotonin can contribute to this damaging excitotoxicity. It occurs when brain receptors called NMDA receptors are activated. Other things besides quinolinic acid can activate NMDA receptors such as glutamate which is abundant in many foods. Most notorious is “monosodium glutamate” or MSG which is used as a taste additive. It has been associated with a feature of excitotoxicity, headache known as the hot dog or Chinese food headache. Many processed foods contain glutamate rich additives, and these compound the brain’s stress response.
Other dietary factors can help quiet NMDA receptors calming the brain including magnesium and zinc. These minerals are often low in depression, and supplementation with good forms is helpful. The use of anti-inflammatory herbs including curcumin from turmeric and resveratrol have been shown to effectively suppress IDO which is the enzyme that causes tryptophan to be converted to quinolinic acid instead of to serotonin. The ketone beta hydroxybutyrate also is effective in quieting inflammation. The immune system’s anti-inflammatory activity also requires omega-3 fatty acids supplementing with significant doses are also helpful.
One of the most overlooked causes of chronic inflammation are food sensitivities, immune inflammatory reactions to components of different foods. Typical of these is that anxiety or depression are often accompanied by digestive symptoms such as abdominal pain, bloating and others. It is important to test for these and restrict inflammatory activating foods.
Natural Treatment of Depression
The treatment of depression is based on addressing the triggering factors discussed above and rebalancing brain activity. Of the above triggering factors stress is the one that is most challenging to resolve. Removing the circumstances that are causing the stress is ideal but impractical in many cases. Things like a bad job can be changed by finding another one. Family, marriage, mortgages and many others tend to be less modifiable. In those situations, teaching the stress reactivity systems in the brain and body to react in a more normal pattern often is the better solution. Several good tools have been developed for that. An effective combination includes vagus nerve stimulation (VNS) and heart rate variability training.
Stress activates the sympathetic or “fight or flight” portion of the nervous system. The system is reset to “rest and repair” by the parasympathetic nervous system of which the vagus nerve is the main branch going between the body and the brain. The nerve has a branch that goes to a specific part of the ear and it is easily stimulated to activate the calming state resetting rest and repair. It has been shown to be effective in reducing inflammation, anxiety and depression making it a great adjunct to stress related disorders.
Summary
Depression is a complex problem with a lot of moving parts. By looking at all of these pieces and putting together a treatment plan that addresses the specific imbalances in each case, natural resolution can be achieved. The pandemic has exacerbated the already large challenge with depression in developed countries. We will need to climb out of this one as we will with all of the other pieces.
- Catherine K. Ettman. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Network Open. 2020;3(9):e2019686.
- Schlaepfer et al. Vagus nerve stimulation for depression: efficacy and safety in a European study Psychological Medicine (2008), 38, 651–661.