BLOG
The Bredesen Protocol™ categorizes the modifiable risk factors that drive the degenerative process involved in Alzheimer’s can be generally divided into 5 groups. Before discussing those it is appropriate to recognize that there are other factors that are involved in the disease process, but they tend to be non-modifiable. The two most important of these […]
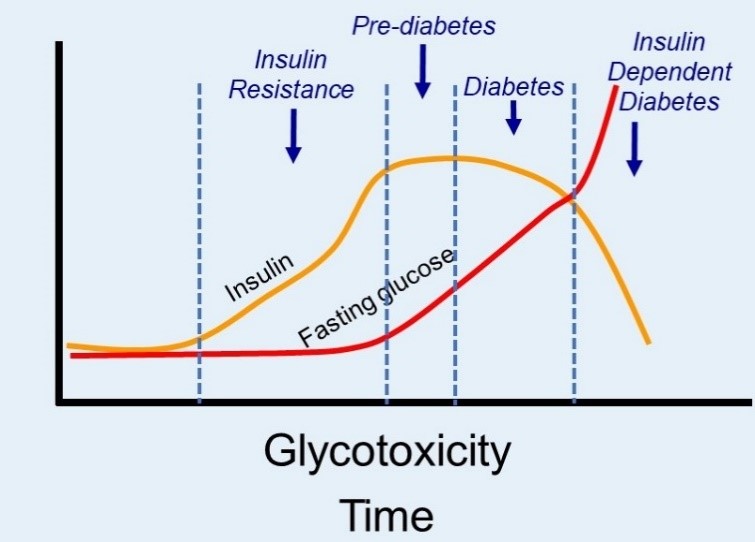
The 5 Dominant Factors that Drive Alzheimer’s