BLOG
Two Expressions of Similar Problems Anxiety and depression are becoming some of the most common chronic illnesses; they are now almost twice as common as heart disease. Of great concern is the frequency of these disorders in adolescents. The Substance Abuse and Mental Health Services Administration released the 2013 statistics which reported that 2.6 million […]
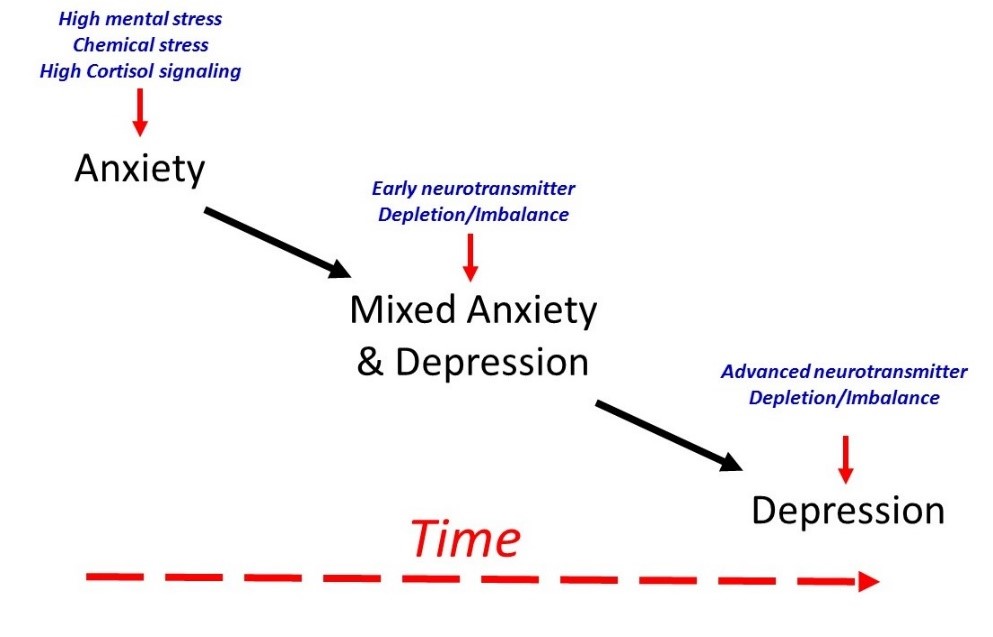
Anxiety, Depression & Mixed Anxiety/ Depression